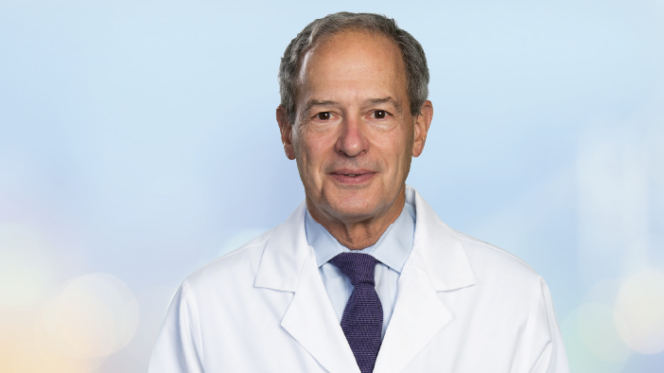
New chief of oncology at Baylor Scott & White Health – North Texas is poised to help cancer patients benefit through greater access to novel research investigating next-generation immunotherapies.
The cancer research and treatment centers of Baylor Scott & White Health provide coordinated care across nearly every cancer, and do so with a multidisciplinary team driven to incorporate advanced therapies and research into patient care. At the heart of the collaborative effort to bring innovative treatments to our patients is Ronan Kelly, MD, MBBCH, MBA, a medical oncologist, clinical researcher, and now one of the anchors of cancer care within the system.
“We are getting closer to our goal of turning cancer into a chronic disease that patients can live with for many years and ultimately reach their normal life expectancy.”
— Dr. Kelly
Pioneering immunotherapy to transform cancer care
As chief of oncology for the organization’s North Texas cancer centers and medical director of oncology for Baylor Charles A. Sammons Cancer Center in Dallas, Dr. Kelly is making it his mission to position the Baylor Scott & White Health cancer center network as a destination for patients seeking advanced immunotherapeutic treatments.
Immunotherapy uses a patient’s immune system to fight cancer. When stimulated to work harder or smarter, the immune system has been found to have the capability to attack cancer and interfere with the ability of tumor cells to grow and spread. This response can often be much more durable than what is achieved with the older chemotherapy regimens oncologists have used for decades.
As a thoracic oncologist and former director of the Gastroesophageal Cancer Therapeutics Program at Johns Hopkins, Dr. Kelly developed an innovative portfolio of clinical trials in lung cancer and gastroesophageal cancer. He continues to lead numerous national and international phase II and phase III clinical trials investigating immunotherapeutic approaches and novel targeted drugs in both cancer types.
Turning cancer into a chronic, manageable condition
“In the early 2000s, the human genome project to map and understand all of the genes that make up human DNA was being completed and I was aware that significant advances were on the horizon for cancer patients,” Dr. Kelly said. “Although we have made amazing strides over the last 15 to 20 years, we have to continue to push forward. With the introduction of immunotherapies, we can harness the inherent cancer-fighting ability of every patient’s immune system. We are getting closer to our goal of turning cancer into a chronic disease that patients can live with for many years and ultimately reach their normal life expectancy.”
Dr. Kelly and his colleagues within the Charles A. Sammons Cancer Center are currently conducting clinical trials through Baylor Scott & White Research Institute that are enrolling patients to investigate next-generation immunotherapeutics, or “living drugs.” Blood is drawn from a patient, and the strongest cancer-fighting immune cells are isolated and genetically altered in the lab to target specific areas of the patient’s cancer. The cells are grown in huge numbers and then given back to the patient as an infusion of “supercharged” immune cells in an attempt to overwhelm the patient’s tumor.
Exciting results have come out of these clinical trials to date across a range of tumor types. For this reason, Dr. Kelly encourages patients to participate in research efforts whenever appropriate. When completed, the American Cancer Society Gene and Jerry Jones Family Hope Lodge in Dallas will support the effort to make important clinical trials available to more patients who live far away.
“Data has shown that patients can potentially do better on a clinical trial than with the standard treatment, but only 2 to 3 percent of American patients participate in clinical trials. We need to get that number up. That’s how we’re going to learn why some people respond to treatment and why some people do not and learn to overcome that resistance. That’s how we’re going to beat cancer,” he added.